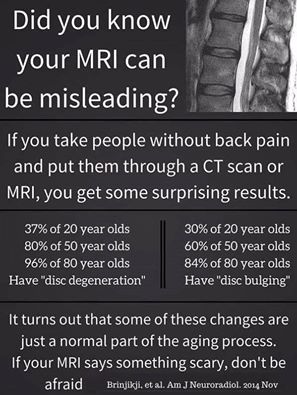
Practitioners and physicians alike are often seeking answers as to why a patient is in pain and will often point to a structural abnormality as the reason for this pain. However, it may surprise you to learn that structural integrity often does not correlate to subjective pain measures in patients. The best example can be seen in a 2015 systematic literature review of imaging features of spinal degeneration in asymptomatic populations.[1]
It turns out that many people have some degree of degeneration or disc bulging without any symptoms, and yet some people have perfect looking backs, but are in a lot of pain.
Rotator cuff disease
The same can be said about rotator cuff injuries. A 2014 meta-analysis comparing the structural integrity after rotator cuff repair with patient function and pain found that functional measures increased and pain levels decreased in patients regardless of the structural integrity of the repair.[2] Patients with intact repairs had higher functional scores in some measures, but no difference in others, and slightly lower pain scores (about 0.9/10 on the visual analog scale) compared with those who had retears. The results of this study suggest that there is not a clinically important difference in validated functional outcome scores or pain for patients who have undergone rotator cuff repair regardless of the structural integrity of the repair. However, patients with intact repairs do have significantly greater strength than those with retears.
Another review published in August 2015 aimed to evaluate the role of the peripheral and central nervous systems in rotator cuff disease.[3] Their review led them to several conclusions.
- RC tendon tears are not necessarily associated with pain or patient-reported loss of shoulder function; however, asymptomatic patients may develop symptoms in a relatively short time.
- 2 recent meta-analyses suggested that patients with intact repairs might not have significant differences in symptom improvement compared with patients with recurrent tears
- Prolonged release of neuropeptides by nociceptive afferent fibers at the dorsal horn may sensitize nocineurons and cause long-term changes in pain processing at the spinal level and higher centers that result in pain hypersensitivity within but also outside the original zone of injury.
- ...sensory abnormalities have been observed on the injured but also on the noninjured side of patients with RC disease, illustrating the involvement of central mechanisms.
These results were also confirmed by a February 2016 pilot study which found that platelet rich plasma (PRP) could reduce the size of rotator cuff tears in some patients.[4] But when they evaluated the correlation between structural changes with pain and function they concluded the following;
...the structural changes to the rotator cuff on MRI did not correlate to the pain or functional improvements demonstrated on self-report questionnaires
What the weight of the current evidence seems to suggest is that pain is complicated and a change in the structural integrity may not increase the patient's quality of life.
Knee Osteoarthritis
Another example of this is in knee osteoarthritis.
A 2014 study evaluated the association between structural changes on MRI and symptoms, function and muscle strength in relation to knee osteoarthritis for 87 women.[5]
- Although MRI-detected cartilage lesions, synovitis/effusion and loose bodies did explain part of the muscle strength variability, results suggest that MRI does not improve the link between joint degeneration and the clinical expression of knee OA.
- MRI contributes less than expected to the understanding of pain and function in knee OA and possibly offers little opportunity to develop structure-modifying treatments in knee OA that could influence the patient'spain and function.
Only when patients with knee osteoarthritis reached an advanced stage marked with severe cartilage loss and inflammation of the synovial membrane did they find a correlation between structural integrity and pain in a separate 2014 study on structural associations of symptomatic knee osteoarthritis.[6] Severe macroscopic chondropathy (cartilage disease) lesions graded as 3 or 4 were present in subjects both with and without symptoms, along with other structural changes. The strongest correlation with symptoms was the presence of synovitis, which is inflammation of the synovial membrane.
These findings on synovitis and knee OA symptoms were confirmed in two separate studies published in June 2016 that assessed the correlation between synovitis and self reported pain.[7][8] The results showed a significant correlation between synovitis and pain scores in patients with knee osteoarthritis. One such study demonstrated the presence of macrophage migration inhibitory factor (MIF), a well known pro-inflammatory cytokine, in synovial fluid and found a strong correlation with self reported pain.
The evidence appears to suggest that inflammation is more likely to be correlated with pain than changes in structural integrity as suggested by a March 2016 study yet again assessing the role of inflammation in symptomatic knee osteoarthritis.[9]
Inflammation, as evidenced by synovitis or effusion, is associated with pain sensitization in knee OA. In contrast, bone marrow lesions (BMLs) do not appear to contribute to sensitization in knee OA. Early targeting of inflammation is a reasonable strategy to test for prevention of sensitization and through this, reduction of pain severity, in knee OA.
The main point of this article is bring attention to the fact that a structural change as evidenced by imaging may or may not be the reason your patient is experiencing pain. It certainly may point you in the right direction, but consider the entire system from the cutaneous nerves and the peripheral nervous system, to the muscles, tendons and ligaments, all the way down to the central nervous system and even the cartilage and bone. But focusing on any one system in isolation may be too narrow of an approach to provide lasting symptomatic relief for your patient.
Meniscus injuries
Meniscus tears can occur following a local trauma or spontaneously due to aging and degenerative processes. An asymptomatic meniscal tear finding on MRI scan is common in normal populations. It ranges from ~5 % in young ages and up to 67 % in older ages.[10] In asymptomatic recreational and higher-level athletes there was an overall prevalence of 27.2% of knees with intrasubstance meniscal damage (grades 1 and 2), and 3.9 % of knees with a tear (grades 3 and 4).[11]
Most surgical meniscus repairs are unnecessary.[10][12] A new study shows that exercise therapy is just as effective for treating meniscus injuries as surgery. A total of 140 patients with meniscus injuries in Norway and Denmark took part in the study. They randomized groups for treatment with either exercise or surgery. Two years later, both groups of patients had fewer symptoms and improved functioning. There was no difference between the two groups. However, those who had exercised had developed greater muscular strength.
Hip Labrum Pathologies
Hip and pelvis pain are relatively common presenting complaints in athletic individuals, comprising 5% to 6% of adult sports injuries.[13] Even when there is a confirmed labral tear, it may not be the cause of the individual’s pain. This was highlighted in a study of asymptomatic collegiate and professional ice hockey athletes, which found labral tears in 56% of the study participants.[14] After 4 years of follow-up, none of the athletes missed time due to the labral pathology.[15]
Forty-five normal population volunteers with no history of hip pain, symptoms, injury, or surgery were recruited for an MRI study. The average age of volunteers was 37.8 years (range, 15-66 years old).[16] Labral tears were identified in 69% of hips, chondral defects in 24%, ligamentum teres tears in 2.2%, labral/paralabral cysts in 13%, acetabular bone edema in 11%, fibrocystic changes of the head/neck junction in 22%, rim fractures in 11%, subchondral cysts in 16%, and osseous bumps in 20%. A strong correlation was seen between participant age and early markers of cartilage degeneration.
A separate study evaluated hips in asymptomatic children aged between 2 and 18 years found a 2% prevalence of labral tears.[17]
Shoulder Labrum Pathologies
When evaluating the labrum in the shoulder similar patterns are seen as in the hip. 19 asymptomatic baseball pitcher draft picks underwent a detailed clinical examination performed before contract signing.[18] Sixty-eight percent (13/19), 32% (6/19), and 21% (4/19) of the baseball pitcher draft picks showed tendinopathy, partial thickness tendon tear of the supraspinatus, and acromioclavicular joint osteoarthritis, respectively. Glenohumeral subluxation, glenoid remodeling, and Bennett lesion were present in 53% (10/19), 79% (15/19), and 21% (4/19) of the subjects, respectively. In asymptomatic baseball pitcher draft picks, MRI frequently shows abnormalities involving rotator cuff tendons, the coracohumeral, inferior glenohumeral, labrum, and osseous structures.
Separately, a total of 21 asymptomatic professional pitchers from a single Major League Baseball (MLB) organization underwent preseason MRIs of their dominant shoulder from 2001 to 2010.[19] The mean age at the time of MRI was 29.04 years (range, 20-39 years). Eleven of 21 pitchers had a rotator cuff tear (RCT): 9 had an articular surface tear (AST), and 2 had a full-thickness rotator cuff tear (FTT). Ten had superior labral anterior posterior (SLAP) tears, and 13 had either anterior or posterior labral tears.
And even in normal populations shoulder pathologies are not uncommon. 51 male subjects who had no symptoms in either shoulder underwent ultrasound scan of the rotator cuff, tendon of the long head of the biceps brachii muscle, subacromial-subdeltoid bursa, acromioclavicular joint, and posterior labrum.[20] Ultrasound showed subacromial-subdeltoid bursal thickening in 78% (40/51) of the subjects, acromioclavicular joint osteoarthritis in 65% (33/51), supraspinatus tendinosis in 39% (20/51), subscapularis tendinosis in 25% (13/51), partial-thickness tear of the bursal side of the supraspinatus tendon in 22% (11/51), and posterior glenoid labral abnormality in 14% (7/51).
REFERENCES
- W. Brinjikji et al. Systematic Literature Review of Imaging Features of Spinal Degeneration in Asymptomatic Populations. AJNR Am J Neuroradiol. 2015 Apr;36(4):811-6. doi: 10.3174/ajnr.A4173. Epub 2014 Nov 27.
- Russell RD, Knight JR, Mulligan E, Khazzam MS. Structural integrity after rotator cuff repair does not correlate with patient function and pain: a meta-analysis. J Bone Joint Surg Am. 2014 Feb 19;96(4):265-71. doi: 10.2106/JBJS.M.00265.
- Bachasson D, Singh A, Shah SB, Lane JG, Ward SR. The role of the peripheral and central nervous systems in rotator cuff disease. J Shoulder Elbow Surg. 2015 Aug;24(8):1322-35. doi: 10.1016/j.jse.2015.04.004.
- Marni Wesner, Terry Defreitas, Heather Bredy, Louisa Pothier, Ziling Qin, Ashley B. McKillop, and Douglas P. Gross. A Pilot Study Evaluating the Effectiveness of Platelet-Rich Plasma Therapy for Treating Degenerative Tendinopathies: A Randomized Control Trial with Synchronous Observational Cohort. PLoS One. 2016 Feb 5;11(2):e0147842. doi: 10.1371/journal.pone.0147842. eCollection 2016.
- Baert IA, Staes F, Truijen S, Mahmoudian A, Noppe N, Vanderschueren G, Luyten FP, Verschueren SM. Weak associations between structural changes on MRI and symptoms, function and muscle strength in relation to knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2014 Sep;22(9):2013-25. doi: 10.1007/s00167-013-2434-y. Epub 2013 Feb 2.
- Laura A Stoppiello, Paul I Mapp, Deborah Wilson, Roger Hill, Brigitte E Scammell, and David A Walsh. Structural Associations of Symptomatic Knee Osteoarthritis. Arthritis Rheumatol. 2014 Nov;66(11):3018-27. doi: 10.1002/art.38778.
- Zhang PL, Liu J, Xu L, Sun Y, Sun XC. Synovial Fluid Macrophage Migration Inhibitory Factor Levels Correlate with Severity of Self-Reported Pain in Knee Osteoarthritis Patients. Med Sci Monit. 2016 Jun 25;22:2182-6.
- Riis RG, Gudbergsen H, Henriksen M, Ballegaard C, Bandak E, Röttger D, Bliddal H, Hansen BB, Hangaard S, Boesen M. Synovitis assessed on static and dynamic contrast-enhanced magnetic resonance imaging and its association with pain in knee osteoarthritis: A cross-sectional study. Eur J Radiol. 2016 Jun;85(6):1099-108. doi: 10.1016/j.ejrad.2016.03.017. Epub 2016 Mar 19.
- Neogi T, Guermazi A, Roemer F, Nevitt MC, Scholz J, Arendt-Nielsen L, Woolf C, Niu J, Bradley LA, Quinn E, Law LF. Association of Joint Inflammation With Pain Sensitization in Knee Osteoarthritis: The Multicenter Osteoarthritis Study. Arthritis Rheumatol. 2016 Mar;68(3):654-61. doi: 10.1002/art.39488.
- Marom, N. Asymptomatic Meniscal Tears. Sports Injuries 2014 Jun; pp1-7. doi: 10.1007/978-3-642-36801-1_70-1
- Beals CT. The Prevalence of Meniscal Pathology in Asymptomatic Athletes. Sports Injuries 2016 Apr; pp1-8. DOI: 10.1007/s40279-016-0540-y
- Nina Jullum Kise, May Arna Risberg, Silje Stensrud, Jonas Ranstam, Lars Engebretsen, Ewa M Roos. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomised controlled trial with two year follow-up. BMJ, 2016; i3740 DOI: 10.1136/bmj.i3740
- Seidenberg PH. Hip Pain in Athletes V When It is Not the Labrum. Curr Sports Med Rep. 2015 Sep-Oct;14(5):373-9. doi: 10.1249/JSR.0000000000000192
- Silvis ML, Mosher TJ, Smetana BS, et al. High prevalence of pelvic and hip magnetic resonance imaging findings in asymptomatic collegiate and professional hockey players. Am. J. Sports Med. 2011;39: 715Y21.
- Gallo RA, Silvis ML, Smetana B, et al. Asymptomatic hip/groin pathology identified on magnetic resonance imaging of professional hockey players: outcomes and playing status at 4 years’ follow-up. Arthroscopy. 2014;30: 1222Y8
- Register B. Prevalence of abnormal hip findings in asymptomatic participants: a prospective, blinded study. Am J Sports Med. 2012 Dec;40(12):2720-4. doi: 10.1177/0363546512462124
- Georgiadis AG. Prevalence of acetabular labral tears in asymptomatic children. J Child Orthop (2016) 10:149–154. DOI 10.1007/s11832-016-0717-9
- Del Grande F. High-Resolution 3-T Magnetic Resonance Imaging of the Shoulder in Nonsymptomatic Professional Baseball Pitcher Draft Picks. J Comput Assist Tomogr. 2016 Jan-Feb;40(1):118-25. doi: 10.1097/RCT.0000000000000327.
- Lesniak BP. Glenohumeral findings on magnetic resonance imaging correlate with innings pitched in asymptomatic pitchers. Am J Sports Med. 2013 Sep;41(9):2022-7. doi: 10.1177/0363546513491093.
- Girish G. Ultrasound of the shoulder: asymptomatic findings in men. AJR Am J Roentgenol. 2011 Oct;197(4):W713-9. doi: 10.2214/AJR.11.6971.